
Family History and Cancer Screening: What to Know
If someone in your immediate family - like a parent, sibling, or child - has had cancer, your chances of developing certain cancers (like breast, lung, or colorectal) can double. For ovarian cancer, the risk can triple.
But here's the good news: understanding your family history can help you take control with personalized screening plans.
Key Takeaways:
- Who’s at higher risk?
- If a first-degree relative had cancer (e.g., breast, lung, colorectal, or prostate), start screenings earlier.
- Multiple relatives or early diagnoses (before age 50) often signal inherited risks.
- When to start screenings:
- Breast cancer: Start mammograms at 30–40 or 10 years before the earliest family diagnosis.
- Colorectal cancer: Begin colonoscopies at 40 or 10 years before a family member’s diagnosis.
- Prostate cancer: Start screenings at 40 or earlier if a relative was diagnosed young.
- Genetic testing helps: About 5–10% of cancers come from inherited mutations. Tests like MyRisk or OncoScreen can identify risks early.
- Tools to stay on track: Use apps like NeverMissHealth or charts like My Family Health Portrait to organize your screenings.
Talk to your doctor about your family’s cancer history, and don’t forget to document key details like diagnosis ages and cancer types. Early action can save lives.
How to make a cancer screening plan
How Family History Affects Cancer Risk
Knowing your family's cancer history is important. Around 20% of Americans face a higher risk of cancer due to their family background, yet over 90% of those with a hereditary risk are unaware of it [3].
Key Family History Risk Factors
Certain family history patterns can increase your cancer risk:
- A parent, sibling, or child with cancer raises your personal risk [1].
- Multiple relatives with cancer, especially on one side of the family, may indicate an inherited syndrome [1][2].
- Cancer diagnosed before age 50 is often linked to hereditary risk [2].
- Ashkenazi Jewish or Eastern European ancestry can also play a role [2].
For example, if a first-degree relative or two second-degree relatives have had colorectal cancer or polyps, you might need a colonoscopy at age 40 (or 10 years before the earliest case in your family). If the results are negative, screenings should happen every five years [1].
Inherited Cancer Types
Some cancers are more likely to be hereditary:
- Colorectal cancer: Family history of polyps, early diagnoses, or multiple cases.
- Breast cancer: Relatives with breast cancer, especially under age 50, or male relatives with this condition.
- Ovarian cancer: Any family history, often linked with breast cancer cases.
- Uterine cancer: Multiple cases in the family, particularly with early-onset.
Certain inherited syndromes are also linked to higher cancer risks:
- HBOC syndrome: Increases the risk of breast, ovarian, advanced prostate, and pancreatic cancers [2].
- Lynch syndrome: Associated with higher risks of colorectal, uterine, and ovarian cancers [2].
Talk to your doctor about your family history to determine the right screening schedule. Genetic counseling might also be a good option to explore [2].
Next, we'll cover how to document your family health history to guide these personalized screening decisions.
Creating Your Family Health Record
Start by collecting basic information about your close relatives. Having a detailed family health record can help guide cancer screening and prevention tailored to your needs.
Steps to Document Family History
Here’s what to include in your family health record:
- The type of cancer each relative was diagnosed with and the age at onset [4].
- Details of cancer-related surgeries, including dates [4].
- Birth and death dates of relatives, along with causes of death and their race/ethnicity [4].
Family gatherings like reunions, holiday dinners, or weddings can be great opportunities to gather this information. Consider these tips:
- Prepare your questions ahead of time.
- Always ask for permission before recording any details, and jot down notes immediately.
- Respect any relative's decision not to share certain information.
- Use family photos or keepsakes to help spark memories.
Risk Assessment Methods
There are tools available to help you organize and share your family health history effectively:
- My Family Health Portrait: This tool allows you to create and export a family tree with health details to share with your healthcare provider [5].
- Family Cancer History Chart: A printable chart that maps out cancer diagnoses across three generations, making it easy to share with medical professionals [6].
If you're adopted or missing key details, provide your healthcare provider or genetic counselor with any known health history and your race/ethnicity. This information can help them recommend the best screening options for you [4].
sbb-itb-f369abd
Custom Screening Plans Based on Family Risk
Using your family's health history and risk assessment, collaborate with your healthcare provider to create a tailored screening plan. This approach may differ from general screening guidelines to better suit your specific needs.
Adjusted Screening Schedules
A strong family history often calls for earlier and more frequent screenings than standard recommendations. Here's how recommendations might shift for certain cancer types [7]:
Breast Cancer Screening
- Women with a first-degree relative diagnosed with breast cancer have a 2 to 4 times higher risk.
- Start mammograms at age 30 or 10 years before the earliest family diagnosis - whichever comes first.
- Individuals with BRCA mutations may begin screening as early as age 25.
Colorectal Cancer Screening
- If a first-degree relative was diagnosed with colorectal cancer before age 45, the risk is over 5 times higher than average.
- Start colonoscopies at age 40 or 10 years before the earliest family diagnosis, whichever comes first.
- For Lynch syndrome, begin colonoscopies between ages 20–25 or 10 years before the youngest diagnosis. Repeat every 1–2 years until age 40, then annually.
Prostate Cancer Screening
- Men with a father or brother affected by prostate cancer face about double the risk.
- Begin annual digital rectal exams and PSA testing at age 40 or 10 years before the earliest family diagnosis, whichever comes first.
The Role of Genetic Testing and Counseling
Genetic testing can identify inherited mutations that influence cancer risk and guide screening plans. Around 5% to 10% of cancers stem from inherited gene mutations [9].
Some advanced genetic testing options include:
- MyRisk: A comprehensive panel for hereditary cancers, including a breast RiskScore. Results are typically available in about two weeks [8].
- OncoScreen: Analyzes 94 genes tied to both common and rare cancers, with results ready in 15–20 days [9].
The American Society of Clinical Oncology (ASCO) advises genetic testing when it impacts medical decisions [9]. MyRisk testing is often covered by insurance, with financial assistance options available [8].
While genetic results don't guarantee cancer, they help you take proactive steps for early detection and prevention.
Use the tools below to stay organized and manage your personalized screening plan effectively.
Tools for Managing Cancer Screening
Once your personalized plan is set, these tools can help you stay organized and on schedule.
NeverMissHealth Screening Tracker
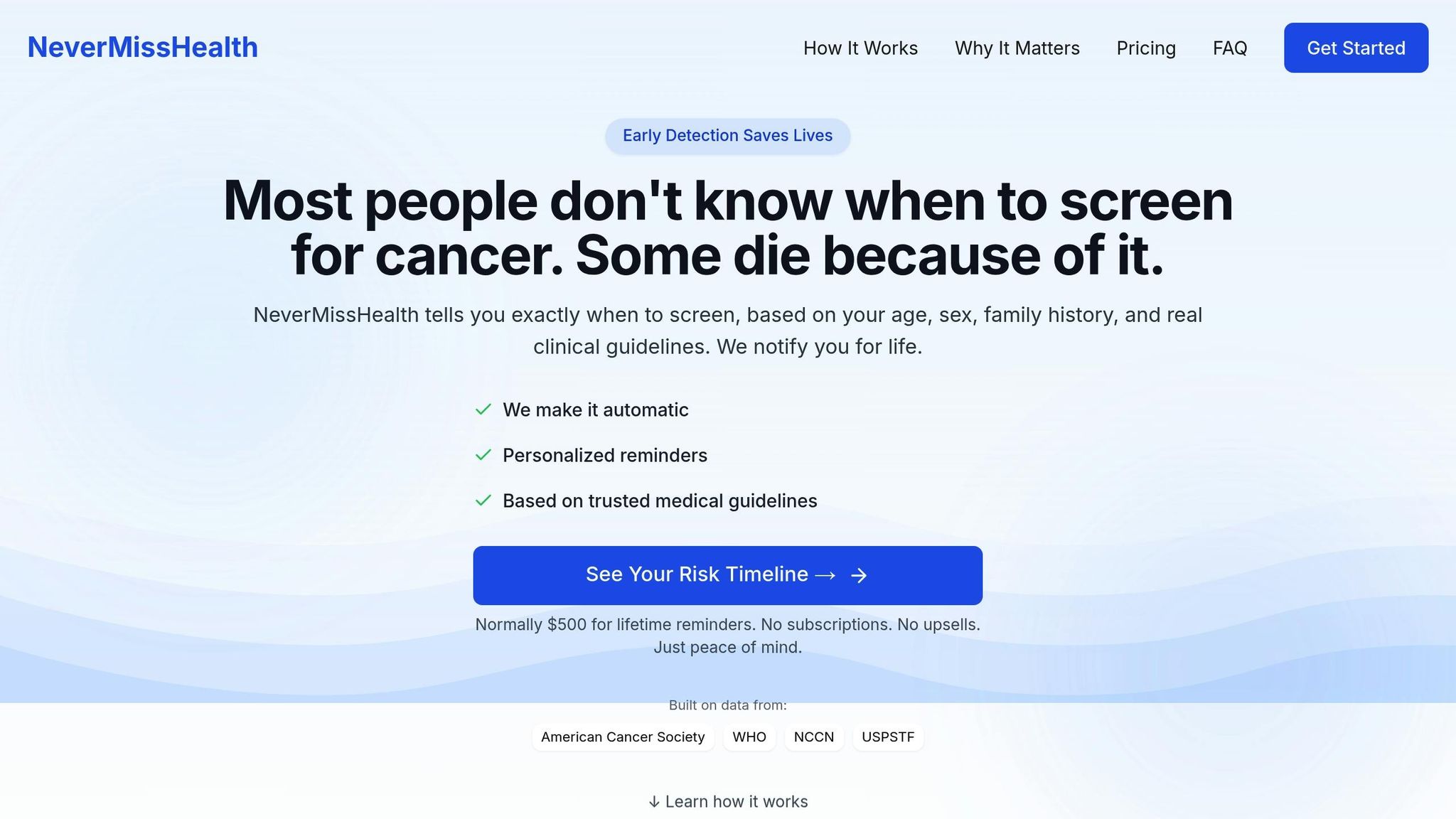
NeverMissHealth offers a Screening Tracker that keeps your plan on track with features like email reminders, calendar syncing, automatic updates to guidelines, and a log of your screening history. Best of all, it doesn’t require any downloads or logins.
Additional Support Services
INHERET provides an automated platform designed to pinpoint hereditary cancer risks, including BRCA and Lynch syndromes. This tool is useful for both patients and healthcare providers, helping facilitate early testing and customized screening plans.
For deeper insights, consider consulting a genetic counselor. They can analyze your family history and provide advice on testing options.
Conclusion: Next Steps for Family Health
To stay on top of your screenings, here are some practical steps to follow:
- Record key details: Include each relative's cancer type, age at diagnosis, and outcome in your family health record.
- Review annually: Go over your family history with your healthcare provider every year to ensure your screening timeline stays accurate.
- Set reminders: Use tools like the NeverMissHealth Screening Tracker to get automated alerts for upcoming screenings.
- Seek expert advice: If you have a complex family history or multiple relatives affected, consider consulting a genetic counselor.
Keep your health records current so your screening plan can adapt as needed.
FAQs
How can I organize my family's cancer history to share with my doctor?
To organize your family's cancer history, start by gathering details about your blood relatives, including any cancer diagnoses, the type of cancer, and the age at diagnosis. If possible, include information about surgeries related to cancer, as well as birth dates, and for deceased relatives, the cause and date of death.
Keep this information in a clear and accessible format, such as a written list or a digital tool. Many find it helpful to use apps or templates designed for family health history tracking. Sharing this organized history with your doctor can help assess your cancer risk and guide personalized screening recommendations. Taking the time to document these details ensures you and your healthcare provider can make informed decisions about your health.
What should I do if my family has a history of cancer?
If your family has a history of cancer, start by gathering as much information as possible about relatives who were diagnosed, including the type of cancer, their age at diagnosis, and how they are related to you. Share this information with your doctor, as it can help determine your risk and guide personalized screening recommendations.
You may also want to discuss genetic counseling with your doctor to assess whether genetic testing is appropriate. This can help identify inherited risks and guide proactive steps like earlier or more frequent screenings. Additionally, adopting healthy lifestyle habits and staying informed about your health can further reduce your cancer risk.
What genetic tests should I consider if cancer runs in my family?
If cancer is common in your family, consulting with a genetic counselor is a great first step. They will review your personal and family health history, create a family tree, and help assess your cancer risk. Based on this evaluation, they may recommend genetic testing to better understand your risks.
Common options include multi-gene panels, which test for several genes linked to cancer, or site-specific testing, which looks for a known mutation identified in a family member. These tests can provide valuable insights and guide personalized cancer screening strategies. Always discuss your options with a healthcare professional to determine what’s best for you.