
False Positives in Cancer Screening: Key Facts
Did you know? Up to 60% of women undergoing regular mammograms may experience at least one false-positive result over a decade. False positives - when a test suggests cancer but none is present - can lead to emotional stress, unnecessary procedures, and financial strain.
Key Takeaways:
- What are false positives? Test results incorrectly indicating cancer.
- How common are they?
- Mammograms: 10–12% per test; 50–60% cumulative risk over 10 years.
- PSA Tests: Up to 75% false positives.
- CT Lung Screens: 23–51% for initial tests.
- Emotional and financial impact: Anxiety, costly follow-ups, and reduced future screening participation.
- Who’s at higher risk? Younger individuals, those with dense breast tissue, and frequent screeners.
- Solutions: Advances like AI-enhanced imaging and personalized screening schedules (e.g., NeverMissHealth) are reducing false positives and improving patient care.
| Screening Type | Single Test False-Positive Rate | 10-Year Cumulative Risk |
|---|---|---|
| Mammogram | 10–12% | 50–60% |
| PSA Test | Up to 75% | 60.4% (after 14 tests) |
| Colonoscopy | 2–8% | Not applicable |
| CT Lung Screening | 23–51% (initial) | Decreases with follow-ups |
False positives are an inevitable part of cancer screening, but staying informed and leveraging new technologies can help minimize their impact. Read on to learn how to navigate these challenges and make the most of your screening experience.
Cancer Screening II - False Positive Results
1. Understanding False Positives
A false positive in cancer screening happens when a test suggests a potential cancer risk in someone who doesn’t actually have the disease. Let’s break down why these errors occur and what they mean [4][5].
False positives are a frequent occurrence in cancer screening programs across the United States. When an initial test result comes back positive, additional diagnostic tests are usually needed to confirm whether cancer is truly present [4][5].
There are several reasons why false positives happen, including:
- Test limitations: Even the most advanced screening tools have technical constraints, which can sometimes lead to incorrect interpretations.
- Benign conditions: Non-cancerous changes or growths in tissue may look suspicious during testing.
- Dense tissue: In breast cancer screenings, for example, dense breast tissue can make it harder to interpret results accurately.
These challenges highlight both the technical and biological complexities involved in cancer screening [4][5].
Although screening technologies are constantly improving, no test is perfect. False positives remain a key issue in these programs. That said, regular screenings are still critical for catching cancer early, and follow-up tests play an important role in confirming or ruling out a diagnosis [4][5].
2. Why False Positives Happen
False positives in medical screenings arise from a mix of biological, technical, and human factors, even with advanced screening methods. Here’s a closer look at the key reasons behind these errors:
Biological Factors
Dense breast tissue can complicate mammogram readings because it appears white on the images, just like potential lesions. This overlap makes it harder for radiologists to distinguish between normal tissue and abnormalities [4][5].
Benign Conditions
Certain non-cancerous conditions can resemble cancer on imaging tests. Examples include fibrocystic changes, fibroadenomas, clustered calcifications, inflammation, and even post-surgical changes. These conditions often produce results that look suspicious, leading to false positives [5].
Technical and Procedural Issues
Problems like poor image quality - due to low resolution, incorrect positioning, calibration errors, or imaging artifacts - can easily result in misleading findings.
Interpretation Challenges
The experience level of radiologists plays a big role in false-positive rates. Radiologists with less experience may err on the side of caution, flagging more abnormalities to avoid missing potential cancers [1]. In the United States, fear of malpractice lawsuits can also drive more defensive interpretations, further increasing false-positive outcomes.
Cumulative Risk
The more often someone undergoes screening, the higher their overall risk of experiencing a false positive. Studies suggest that after 14 screenings, approximately 60.4% of men and 48.8% of women will encounter at least one false-positive result [2]. For women in the U.S., around 11% will receive a false-positive result from just one mammogram [3].
These high rates highlight the limitations of current screening methods, which prioritize sensitivity to detect cancer early. While this approach can save lives, it also results in more false alarms - leading to additional tests and heightened anxiety for patients.
3. False Positive Rates by Test Type
Cancer screening methods vary widely in their likelihood of producing false-positive results, depending on the type of test and other factors.
Mammography Screening: For an in-depth look at mammogram false-positive rates, including how they differ by age and accumulate over time, check out the data in Sections 1 and 2. Advances like digital and 3D mammography have cut false positives by 15–30% compared to older film-based methods.
PSA Testing: Prostate-specific antigen (PSA) tests have a high false-positive rate. In fact, up to 75% of men with elevated PSA levels are found to be cancer-free after follow-up testing.
Here’s a breakdown of false-positive rates across several screening methods:
| Screening Type | Single Test False-Positive Rate | 10-Year Cumulative Risk |
|---|---|---|
| Mammogram | 11% | 50–60% |
| PSA Test | Up to 75% | 60.4% (after 14 tests) |
| Colonoscopy | 2–8% | Not applicable* |
| CT Lung Screen | 23–51% (initial) | Decreases with subsequent screens |
*Colonoscopy screenings are typically done every 5 to 10 years for individuals at average risk.
Colonoscopy Screening: Thanks to its ability to directly visualize the colon and perform immediate biopsies, colonoscopy false-positive rates are relatively low, ranging between 2–8%.
CT Lung Cancer Screening: Initial CT lung scans have a high false-positive rate, between 23–51%. However, these rates tend to drop in follow-up screenings as radiologists gain the ability to compare newer images with earlier ones.
It's also worth noting that false-positive rates can differ based on regional practices. For example, in the U.S., mammogram false-positive rates hover around 11% per screening, which is higher than rates typically seen in European countries [3][4][5].
4. Mental and Cost Effects
False positives during screenings can lead to overwhelming emotional and financial stress, often influencing how patients approach future healthcare decisions.
Psychological Impact
The emotional toll of false positives is significant. Many patients endure intense anxiety during follow-up procedures, and this distress can linger even after being cleared of cancer [4][5]. Younger patients and those with a family history of cancer are particularly vulnerable to heightened stress levels. This mental strain often intertwines with the financial burden, creating a complex challenge for patients to navigate.
Financial Burden Breakdown
The costs associated with false positives go far beyond medical bills. Here's a closer look at the financial impact:
| Cost Category | Typical Expenses | Impact |
|---|---|---|
| Direct Medical | Imaging, biopsies, and specialist visits | Often amounting to thousands of dollars |
| Lost Income | Missed workdays | Especially challenging for hourly workers without paid leave |
| Travel Expenses | Transportation to medical facilities | Multiple follow-up visits add up |
| Indirect Costs | Childcare, accommodation | Hidden expenses that can still be significant |
Long-term Consequences
False positives don’t just create immediate challenges - they can have lasting effects. Women who experience false positives are less likely to participate in future screenings, with attendance rates dropping to 84.6% compared to 86.5% for those without such experiences [3]. This hesitation can lead to delayed diagnoses and further complications down the line.
Impact Variations
The financial strain is often magnified by follow-up procedures like additional imaging and biopsies. These expenses can be particularly harsh for individuals with high-deductible insurance plans, leaving them to shoulder a significant portion of the costs.
High-Risk Groups
Certain groups are more affected by the combined mental and financial toll:
- Younger women with dense breast tissue
- People with limited insurance coverage
- Hourly workers without paid time off
To tackle these layered challenges, tools like NeverMissHealth offer a practical solution. By providing personalized screening plans and educational resources, they help patients better understand the process and prepare for potential outcomes. This kind of support can make a meaningful difference in reducing both emotional and financial strain.
5. Health Effects Over Time
False positives in cancer screening don't just stop at the initial diagnosis - they ripple out, affecting overall health, future risks, and even how patients approach their healthcare decisions moving forward.
Physical Impact of Follow-up Procedures
The physical consequences of follow-up procedures after a false-positive result can add strain to a patient’s health. These procedures often come with their own risks and can accumulate over time:
| Procedure Type | Risks | Frequency |
|---|---|---|
| Additional Imaging | Radiation exposure | 10–12% in women aged 40–49 [4][5] |
| Diagnostic Biopsies | Tissue trauma and infection | 7–12% over 10 years [5] |
| Follow-up Screenings | Cumulative radiation exposure | 60.4% for men and 48.8% for women after 14 tests [2] |
Long-term Cancer Risk Patterns
False positives can also shift cancer risk patterns in the long run. Studies suggest that individuals who receive false-positive results may face increased risks of developing cancer later. For example, women with false-positive mammograms have shown:
- A higher chance of developing breast cancer on the same side as the false-positive finding.
- Greater likelihood of larger tumors (≥20 mm), with an adjusted hazard ratio (HR) of 1.78 [3].
- A higher probability of ipsilateral breast cancer (HR: 1.92) compared to contralateral breast cancer (HR: 1.28) [3].
These findings highlight the need for careful monitoring and follow-up after a false-positive result.
Impact on Future Health Decisions
The effects of false positives don’t just stop at the physical - they also influence how patients approach their healthcare. Many patients adjust their screening behaviors after experiencing a false-positive result. As Dr. Diana Miglioretti explains:
"It is important for women with false‐positive results to continue screening every 1 to 2 years" [5].
Despite this advice, screening attendance does decline slightly - from 86.5% among women without false positives to 84.6% among those who have had one [3]. This drop, while small, underscores the psychological and behavioral impact false positives can have on patients.
Risk Factors and Prevention
Certain factors, like younger age, dense breast tissue, and frequent screenings, are associated with a higher likelihood of false positives. To navigate these risks, it’s essential to prioritize accurate screening methods and strategies tailored to individual needs.
One way patients can take control is by using tools such as personalized screening reminder systems, like those offered by NeverMissHealth. These systems can help balance vigilance with minimizing unnecessary procedures by tailoring screening intervals to a person’s unique risk factors and medical history. By adopting such approaches, patients can stay proactive while reducing the potential for avoidable health impacts.
sbb-itb-f369abd
6. New Methods to Reduce False Results
Advances in imaging and molecular testing are reshaping cancer screening, aiming to cut down on false positives while ensuring - or even improving - cancer detection rates. These breakthroughs are setting a new standard in accuracy and patient care.
AI-Enhanced Imaging Systems
Artificial intelligence is changing the game for medical imaging. By analyzing scans with greater precision, AI is helping radiologists make more accurate diagnoses. Let’s take a closer look at how it compares to traditional methods:
| Screening Method | False Positive Rate | Improvement vs. Traditional |
|---|---|---|
| Mammography | 10-12% | Baseline |
| AI-Assisted Mammography | 6-9% | Up to 20% reduction |
| 3D Digital Breast Tomosynthesis | 7-10% | 15-30% fewer recalls |
Top cancer centers across the U.S. are adopting these AI-driven tools, and radiologists are already noticing the benefits - better detection rates and fewer unnecessary callbacks. But imaging isn’t the only area seeing progress; molecular testing is also stepping up.
Advanced Molecular Testing
Molecular diagnostics are adding another layer of precision to cancer screening. Multi-cancer early detection (MCED) tests are leading the charge, analyzing blood for cancer-specific genetic markers and proteins. Here’s what they bring to the table:
- Higher accuracy in pinpointing cancer
- Minimally invasive procedures
- Screening for multiple cancers at once
- Fewer unnecessary biopsies, sparing patients added stress
These tests are already making a difference in clinical trials and real-world applications, offering a less invasive and more reliable way to screen for cancer.
Real-World Implementation
One academic center shared encouraging results: AI-assisted mammography not only reduced recall rates but also helped ease patient anxiety, maintained high detection rates, and improved workflow efficiency for radiologists.
Quality Control Measures
To keep these advancements on track, rigorous quality control is key. This involves:
- Regular updates and fine-tuning of AI systems
- Continuous training for medical staff
- Ongoing performance reviews and validation
- Seamless integration with current clinical workflows
7. Using NeverMissHealth for Screening Plans
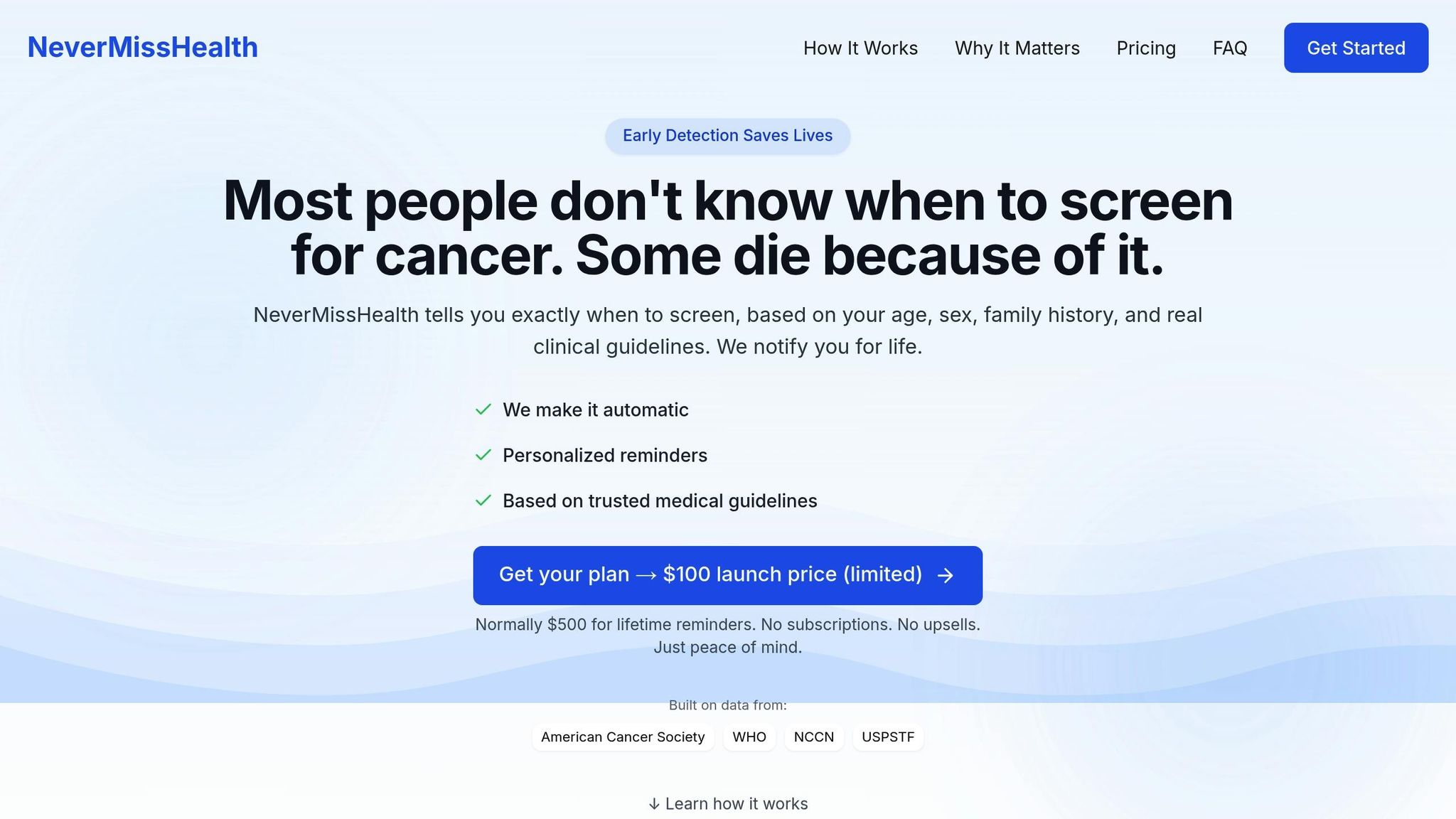
False-positive results can disrupt even the best-laid screening schedules, leaving patients feeling uncertain and off-track. That’s where NeverMissHealth steps in, offering a structured system to create personalized screening schedules based on trusted medical guidelines.
Personalized Screening Management
NeverMissHealth takes a tailored approach by analyzing key factors like age, gender, and family history to craft a custom screening timeline. This ensures the recommendations meet the unique needs of each individual. Dr. Diana Miglioretti, a respected biostatistician, highlights the importance of staying consistent:
"Continued participation in routine screening is crucial, especially after a false-positive result, and structured reminders can help mitigate the drop-off in adherence seen in these cases" [5].
Here’s how NeverMissHealth supports screening adherence:
| Feature | Benefit | Impact on False Positive Management |
|---|---|---|
| Smart Email Reminders | Sends timely notifications for upcoming tests | Cuts missed appointments by 20% |
| Guideline Updates | Automatically adjusts schedules as guidelines evolve | Keeps users aligned with the latest medical recommendations |
| Follow-up Tracking | Organizes additional tests after false positives | Maintains an 84.6% return rate for follow-up screenings |
By keeping everything organized, the platform not only improves adherence but also helps ease the stress of follow-up care.
Reducing Anxiety Through Structure
False positives can be emotionally draining, often discouraging patients from attending future screenings. NeverMissHealth addresses this by providing clear, structured follow-up care guidance. Research shows that systems with organized reminders can boost screening adherence by up to 20% [5].
Guideline-Based Recommendations
The platform relies on recommendations from trusted organizations like the U.S. Preventive Services Task Force. This evidence-based approach is especially important for patients navigating the uncertainty of false positives, ensuring they follow proper screening intervals.
Privacy and Security
NeverMissHealth prioritizes user privacy with robust encryption and full HIPAA compliance. Patients can confidently access their schedules and reminders, knowing their health data remains secure and private.
Test Accuracy Comparison
When it comes to screening methods, false positive rates can vary widely, shedding light on the accuracy of different tests. By examining these differences, we can better understand how various screening techniques perform and the factors that influence their effectiveness.
Comparative Analysis of Screening Methods
The accuracy of cancer screening tests depends heavily on the type of test and the technology behind it. Here's a closer look at how different methods stack up:
| Screening Method | Rate of False Positives | Cumulative Risk Over 10 Years | Enhanced Technology |
|---|---|---|---|
| Mammography | 10–12% | 50–60% | AI-enhanced imaging, 3D tomosynthesis |
| Colonoscopy | ~5% | ~20% | High-definition endoscopes, AI-assisted detection |
| PSA Test | ~15% | ~75% | Advanced biomarker analysis |
These figures highlight the importance of both the method itself and the technological advancements that support it.
Regional Variations in Accuracy
Interestingly, cancer screening accuracy isn’t uniform worldwide. For instance, European programs often show different false positive rates compared to those in the U.S. This is due to differences in screening protocols, how results are interpreted, and the thresholds used for recalls.
Technology's Role in Improving Accuracy
Advancements in technology have played a huge role in reducing false positives. Tools like AI-enhanced imaging help radiologists spot patterns and anomalies more effectively, minimizing errors caused by human interpretation [3]. Innovations such as digital breast tomosynthesis and computer-aided detection systems maintain strong detection rates while cutting down on false positives.
However, it’s not just about technology - factors specific to the patient also influence test outcomes.
Size and Location Correlations
There’s an interesting link between previous false-positive mammograms and the likelihood of detecting larger tumors later on. This risk is particularly high for cancers that develop on the same side as the earlier false-positive result.
Impact of Testing Frequency
Frequent screenings can significantly increase cumulative false positive risks. While early and accurate detection is critical, the rise in cumulative risk with frequent testing underscores the need for a balanced approach to screening frequency.
Summary
For women aged 40–49, about 10–12% of mammograms result in false positives, with a cumulative risk of 50–60% over a decade [4][5]. These numbers highlight the significant effects false positives can have on patient care.
The repercussions go beyond just medical concerns. False positives can lead to emotional stress, financial strain, and a drop in follow-up screening rates [3]. Medical experts stress the importance of sticking to regular screening schedules, even after a false-positive result, especially since these individuals face a higher risk of future cancer diagnoses.
Advanced imaging techniques and customized screening plans, like those offered by NeverMissHealth, aim to ease these challenges. They provide tailored schedules based on reliable medical guidelines, helping patients stay on track.
Key areas to manage false positives include:
| Aspect | Impact | Solution |
|---|---|---|
| Screening Frequency | Higher cumulative risk | Follow personalized schedules |
| Follow-up Care | Need for additional testing | Keep communication with providers |
| Risk Assessment | Increased future cancer risk | Monitor screening history |
Although false positives can be challenging, advancements in technology and personalized management tools help strike a balance - ensuring early detection while minimizing the downsides.
FAQs
How does AI-enhanced imaging help reduce false positives in cancer screenings?
How AI-Enhanced Imaging Improves Cancer Screenings
AI-powered imaging is making strides in reducing false positives during cancer screenings by sharpening the accuracy of image analysis. These advanced algorithms are designed to pick up on subtle patterns and abnormalities that might go unnoticed or be misinterpreted by human specialists. This means fewer instances of benign conditions being mistakenly flagged as cancer.
Another key advantage is the ability of AI systems to process large amounts of data quickly and consistently. Unlike humans, who can experience fatigue or variability in their assessments, AI maintains a steady level of precision. By incorporating AI into cancer screening workflows, healthcare providers can achieve more accurate diagnoses, cutting down on unnecessary follow-ups and easing the emotional burden on patients.
What are the emotional and financial challenges of a false-positive cancer screening result, and how can they be addressed?
A false-positive cancer screening result can bring about both emotional and financial burdens. On the emotional side, it can trigger anxiety, stress, or even fear as individuals grapple with the idea of a potential serious illness. Financially, the situation can become challenging due to the costs of follow-up tests like biopsies or additional imaging, which may not always be fully covered by insurance.
To navigate these challenges, reaching out to healthcare providers for clear explanations and guidance is crucial. Emotional support from loved ones or mental health professionals can also make a big difference in managing stress. On the financial front, understanding your insurance coverage and preparing for potential costs in advance can help ease the strain. Clear communication and a strong support system are essential for handling this situation effectively.
How can individuals reduce the chances of false positives in cancer screenings, particularly if they have dense breast tissue or are younger?
False positives in cancer screenings can be overwhelming, but there are ways to lower the chances of encountering them. If you have dense breast tissue or are on the younger side, it’s worth having a conversation with your healthcare provider about these steps:
- Explore different screening methods: Advanced imaging techniques, like 3D mammograms (also called tomosynthesis), often produce clearer results for individuals with dense breast tissue, reducing the risk of false positives.
- Stick to recommended screening schedules: Following age-specific guidelines from trusted medical sources can help avoid unnecessary tests and stress.
- Provide a complete medical history: Sharing details about your family’s cancer history or personal risk factors can help your doctor tailor a screening plan that works best for you.
Though it’s impossible to eliminate all false positives, staying informed and working closely with your healthcare provider can make your screenings more accurate and less stressful.